Communication and patient partnership
Knowledge
Objective Activity
Osteopathic Practice Standards
Patient feedback
Skills and Performance
Building positive patient relationships
Osteopath and university course leader Diana Pitt shares her learning and insights into gathering patient feedback, and how she applied this to improve her service and grow her practice
Diana Pitt graduated from the European School of Osteopathy in 1988 and later took an MSc in Research Methods (1995) and a Teaching Qualification PGCAP in 2014.
Diana ran her own multidisciplinary clinic in Kent from 1996 to 2013, relocating to Yorkshire to work for Leeds Beckett University. She now works one-and-a half days a week in clinical practice in York and is also the Course Leader for the MSc Pre-Registration Osteopathy at the University College of Osteopathy.
Which aspect of your practice did you decide to get feedback on?
The information I hoped to obtain was feedback about my ability to build positive patient relationships. I’m always giving feedback to students and encouraging them to receive feedback, and felt it was important to be in that situation myself too! It’s very easy to think that we listen to patient feedback, but do we really? Do we hear what we want to and not what people are actually thinking or saying to us?
Why did you choose this aspect to explore?
I had several reasons for doing this: I’m interested in how we come across to our patients because we have to adapt to all different types of people and their individual needs and problems. It’s difficult to see one’s own behaviour through our own eyes, and receiving feedback from patients is a valuable way of gaining insight into how they see our communication and behaviours.
I also know from observing clinical students over many years that having excellent communication skills is an extremely important factor in gaining patient confidence in the treatment you are giving and encouraging ‘compliance’ with self-care advice, etc.
Which method did you use to gather feedback?
I decided to use the CARE patient feedback measure, which has been validated and widely used for 10 generic cross-professional aspects of patient care (caremeasure.org/about.php). For example, the patient is asked to rate how well you ‘let them tell their story’. It’s simple to complete by using tick boxes for a range of responses, with the useful addition of a free text box for any comments which patients wish to make.
I printed out 30 questionnaires and stapled a simple covering letter to each of them. The letter explained that responding to the questionnaire was entirely voluntary and completely anonymous. I asked them to post the completed form through our practice front door letter box (this was not overlooked in any way by staff or patients). I also reassured them that there would be no follow-up but that we might use the data for marketing on our website.
How long did it take?
It took six weeks to give the questionnaire to 30 patients who were willing to complete it. I waited two months to make sure I received as many questionnaires back as possible before analysing the results.
How did you analyse the feedback?
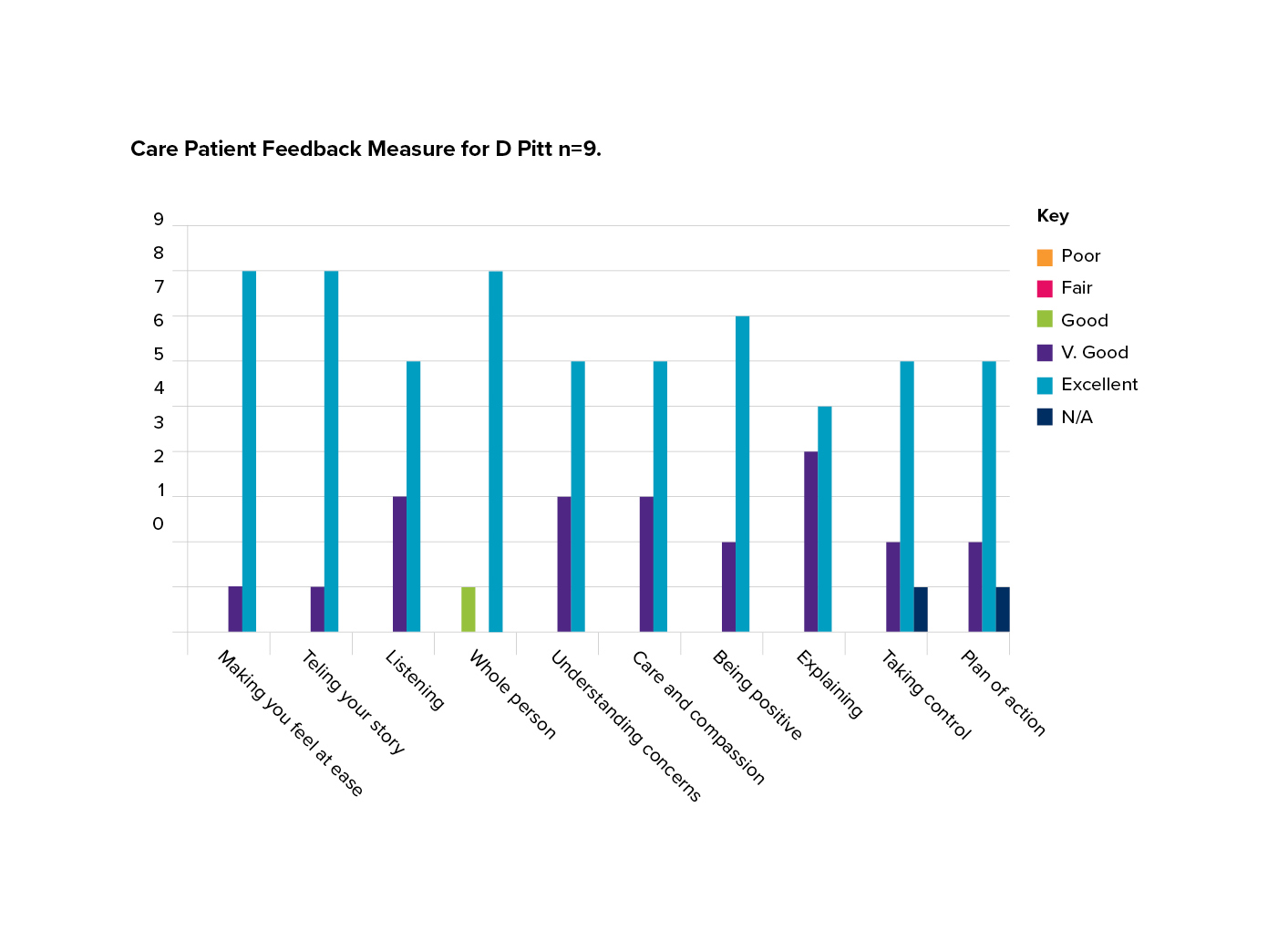
I received nine completed questionnaires, so the numbers were small, and I used a very simple tally system to record the scores which were on a six-point Likert-type scale for the 10 questions. Then I put the scores for each question on a simple bar chart in Excel (see below). This made the results very easy to view. The free text was analysed separately by looking for broad themes.
After reflecting on the results, what were the learning points for you?
I had good feedback in most areas – mainly excellent – which was reassuring.
Particular strengths were:
- Making the patient feel at ease
- Letting the patient tell their story
- Seeing the patient as a whole person
- Being positive.
However, I had a few responses in the ‘very good’ category and I was surprised that two respondents didn’t think that ‘having an action plan’ and ‘allowing the patient to take control’ were applicable to their problem. This did make me alter my practice and set aside specific time within a consultation to really explain the management plan and what their part in it is, to help patients take better control of their symptoms and management.
In terms of the method I used to collect feedback, I thought the response rate would be greater because I opted to give the form out in person. I believe some practitioners in our support/study group had a better response rate from online questionnaires, so I may try this in the future, so that I can compare results across the years.
Did you link the learning with the themes of the Osteopathic Practice Standards?
I linked this learning with:
Theme A: Communication and patient partnership.
But it also links to:
Theme B: Knowledge, skills and performance.
as I have learned more about undertaking patient feedback and analysis.
See: standards.osteopathy.org.uk
Would you gather patient feedback again?
Yes, it helps keep me reflective and ensures that I’m continuing to provide a good service to patients and adhering to practice standards. Ultimately, data like this may help with practice-building too, and could be used for marketing on the practice website.